Oral and Inactivated Poliovirus Vaccines
I will begin my blog post by explaining the difference between the IPV, or the inactivated poliovirus vaccine and the OPV, or the oral poliovirus vaccine. Interestingly enough, we will see how the combination of these two vaccines has been used to protect people the most efficiently around the world. According to a chapter in Nester’s Microbiology Textbook, the Salk vaccine, which is now known as the IPV, was developed in the 1950’s which requires multiple injections to receive full protection. This vaccine contains inactivated particles of all three serotypes of the poliovirus. The Sabin vaccine, now know as the OPV was developed in 1961 and uses attenuated strains of the poliovirus to provide immunity. The advantage of this vaccine is its lowered price in comparison with the IPV. To ensure herd immunity, the OPV must be used because of its ability to induce mucosal immunity in the throat and intestinal tract. However, very rarely vaccine-related poliomyelitis (the disease caused by poliovirus) will occur in people receiving the OPV, so it has been phased out in many countries that have achieved eradication. In places where wild-type poliovirus is still present, the OPV is commonly used.

Poliovirus in the United States
According to an article by the CDC, in June of 1996, the ACIP, or the advisory committee on immunization practices, recommended a switch from only OPV vaccination to OPV and IPV vaccination so as to avoid rare, but deadly, vaccine-related poliomyelitis from the OPV vaccines. The last case in the United States from a residing person was in 1979. In the entire Western Hemisphere, the poliovirus was eradicated due to steady immunization from the OPV. In 2000 began the recommendation to use only the IPV in the United States as long as population immunity remained high (through herd immunity) and prevention of importation. Vaccination among children in the United States remains high due to immunization initiatives, particularly by the World Health Organization and other organizations within the United States. Vaccination of children is so important because it will not only affect the child, but also those around them. According to an article from Kidshealth.org, children should receive the IPV in the United States at ages 2 months, 4 months, 6-18 months, and 4-6 years.
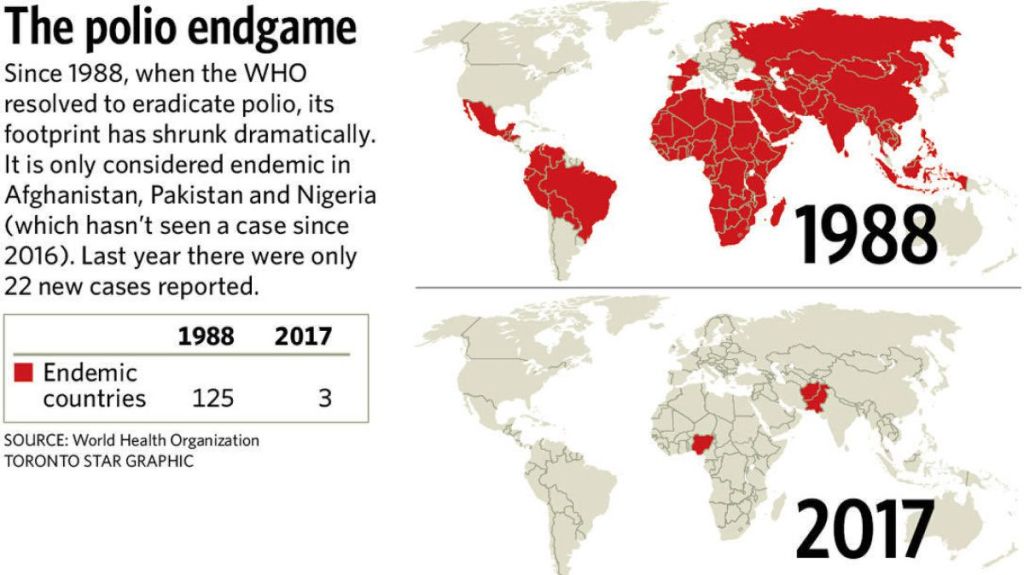
Poliovirus Around the World
According to an article in the Bangladesh Journal of Medicine, the oral polio vaccine, or OPV, has been one of the main defenses against in India for the past 30 years. In the last two years however, the IPV or the inactivated polio vaccine is rising in popularity, now acting as the main protection in immunity against the type 2 poliovirus as indigenous poliovirus outbreaks declines. According to an article in The Lancet, vaccine-derived cases of the poliovirus have occurred recently in parts of Africa and the Philippines and an upsurge in cases of the wild-type poliovirus in Pakistan and Afghanistan. I think that hygienic practices and sanitation standards in many parts of the world could also be used to mitigate outbreaks of the poliovirus. I think that the right to water and sanitation can be drawn upon in these areas of the world by citizens to further protect themselves from the virus when the vaccine is less accessible. Health in populations starts at the government and I believe vaccines as well as sanitation fall under government responsibility.